Introduction to Transcranial Magnetic Stimulation (TMS)
Depression is a highly prevalent mental health condition that can profoundly impact quality of life and daily functioning. For many, traditional treatments such as antidepressant medications and psychotherapy may not offer sufficient relief or may carry undesirable side effects. The procedure utilizes magnetic fields to stimulate nerve cells in specific regions of the brain responsible for mood regulation. Many patients seeking personalized guidance on TMS and other advanced mental health therapies can find valuable resources and support at brainhc.com, where experts provide information on treatment options, clinic locations, and ongoing care strategies. With mounting research supporting its effectiveness and safety, TMS is rapidly changing the treatment landscape for depression. Patients often report noticeable improvements in mood, energy levels, and overall quality of life after undergoing TMS therapy. Accessing professional support early can make a significant difference in achieving lasting mental health benefits.
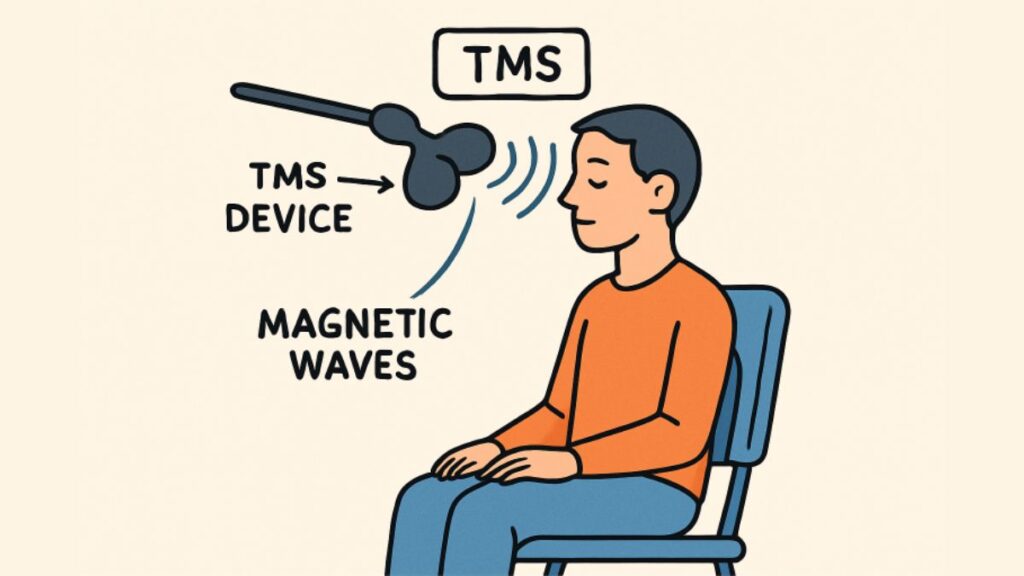
How TMS Works
Transcranial Magnetic Stimulation (TMS) uses electromagnetic induction to stimulate specific areas of the brain. During treatment, a device places a magnetic coil against the patient’s scalp, typically near the forehead. The coil generates magnetic pulses that pass painlessly through the skull and reach targeted brain regions. These pulses focus on areas involved in mood regulation, such as the dorsolateral prefrontal cortex, helping activate brain circuits that may be underperforming in people experiencing depression. For those interested in learning more about TMS, US News offers a detailed guide on how the therapy works, its potential benefits, and what patients can expect during treatment. Because TMS is non-invasive, it doesn’t require surgery or anesthesia, making it a suitable option for people who prefer less intensive interventions. Sessions generally last 20-40 minutes and are usually scheduled daily over several weeks, depending on the individualized treatment plan.
Effectiveness of TMS in Treating Depression
A growing body of scientific evidence supports the effectiveness of TMS. In several large-scale studies, TMS has demonstrated significant reductions in depressive symptoms, even among individuals who have not responded to multiple medication trials. The positive outcomes associated with TMS are helping to reshape clinical guidelines and expand the tools available to mental health providers in treating persistent and treatment-resistant depression.
Advantages Over Traditional Treatments
- Non-Invasive: TMS does not involve surgery, anesthesia, or the placement of implanted electrodes, setting it apart from other neuromodulation options like deep brain stimulation or vagus nerve stimulation.
- Minimal Side Effects: The procedure is generally well-tolerated. The most common side effects are mild headaches or scalp discomfort, which usually resolve soon after sessions and diminish over time.
- Rapid Onset of Action: Many patients notice meaningful improvements within the first few weeks, sometimes even in the first week of treatment.
- No Systemic Effects: Unlike medications, TMS does not circulate through the bloodstream, thereby dramatically reducing the risk of systemic side effects such as weight gain, sexual dysfunction, or gastrointestinal disturbances.
- Compatible with Other Treatments: TMS can be used alongside ongoing therapy or medication under medical supervision, allowing for integrated treatment plans.
Long-Term Benefits
One of the most appealing aspects of TMS is the duration of its therapeutic benefits. Research has shown that symptom relief can persist for months or even longer after a completed course of treatment. For instance, MRI-guided TMS was reported by Neuroscience News to sustain significant improvements in both depression and anxiety for up to six months post-treatment.
Continued monitoring and periodic “maintenance” sessions may be recommended for some individuals, allowing flexibility based on clinical response and personal needs. The durability of this effect stands as a notable advantage compared to some other treatment approaches, where relapse rates can be higher.
Considerations and Eligibility
Not everyone with depression will be a good candidate for TMS therapy. Factors influencing eligibility include the type and duration of depression, previous treatment history, the presence of metal implants or certain health conditions, and individual risk factors. As with all medical interventions, a thorough evaluation by a qualified mental health professional is essential to determine suitability, discuss potential advantages and risks, and establish a collaborative treatment plan tailored to the patient’s unique circumstances. Consultation with your healthcare provider will ensure that any underlying health concerns, medication interactions, or other contraindications are carefully reviewed before initiating TMS therapy.
Conclusion
Transcranial Magnetic Stimulation stands at the forefront of modern depression management, offering new hope for individuals who have struggled to find relief from standard therapies. Its strong safety profile, rapid impact, minimal disruption to everyday life, and sustained improvements position TMS as an exceptionally valuable option in the spectrum of mental health care. Continued research will only expand our understanding of TMS and its broader applications in neuropsychiatric care. For anyone considering next steps in managing depression, discussing the suitability of TMS with a specialized provider is a proactive and promising move toward lasting wellness.